Press Releases
January 5, 2017– A steady decline over more than two decades has resulted in a 25% drop in the overall cancer death rate in the United States. The drop equates to 2.1 million fewer cancer deaths between 1991 and 2014.
The news comes from Cancer Statistics 2017, the American Cancer Society’s comprehensive annual report on cancer incidence, mortality, and survival. It is published in CA: A Cancer Journal for Clinicians and is accompanied by a consumer version of the publication, Cancer Facts and Figures 2017.
The report estimates that in 2017, there will be 1,688,780 new cancer cases and 600,920 cancer deaths in the United States. Over the past decade of available data, the overall cancer incidence rate was stable in women and declined by about 2% per year in men, while the cancer death rate declined by about 1.5% annually in both men and women.
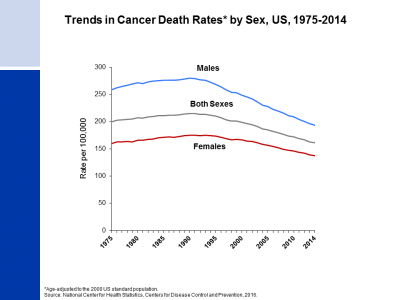
The cancer death rate dropped from its peak of 215.1 (per 100,000 population) in 1991 to 161.2 (per 100,000 population) in 2014, the latest year for which data was available to analyze. The drop is the result of steady reductions in smoking and advances in early detection and treatment, and is driven by decreasing death rates for the four major cancer sites: lung (- 43% between 1990 and 2014 among males and -17% between 2002 and 2014 among females), breast (-38% from 1989 to 2014), prostate (-51% from 1993 to 2014), and colorectal (-51% from 1976 to 2014).
The report also finds significant gender disparities in incidence and mortality. For all sites combined, the cancer incidence rate is 20% higher in men than in women, while the cancer death rate is 40% higher in men.
The gender gap in cancer mortality largely reflects variation in the distribution of cancers that occur in men and women, much of which is due to differences in the prevalence of cancer risk factors. For example, liver cancer, a highly fatal cancer, is three times more common in men than in women, partly reflecting higher Hepatitis C virus infection, historical smoking prevalence, and excess alcohol consumption in men. The largest sex disparities are for cancers of the esophagus, larynx, and bladder, for which incidence and death rates are about 4-fold higher in men. Melanoma incidence rates are about 60% higher in men than in women, while melanoma death rates are more than double in men compared to women.
Racial disparities in cancer death rates continue to decline. The excess risk of cancer death in black men has dropped from 47% in 1990 to 21% in 2014. The black/white disparity declined similarly in women, from a peak of 20% in 1998 to 13% in 2014. Although the cancer death rate remained 15% higher in blacks than in whites in 2014, increasing access to care as a result of the Patient Protection and Affordable Care Act may expedite the narrowing racial gap. From 2010 to 2015, the proportion of blacks who were uninsured dropped in half, from 21% to 11%, as it did for Hispanics (31% to 16%). Gains in coverage for traditionally underserved Americans will facilitate the broader application of existing cancer control knowledge across every segment of the population.
“The continuing drops in the cancer death rate are a powerful sign of the potential we have to reduce cancer’s deadly toll,” said Otis W. Brawley, M.D., FACP, chief medical officer of the American Cancer Society. “Continuing that success will require more clinical and basic research to improve early detection and treatment, as well as creative new strategies to increase healthy behaviors nationwide. Finally, we need to consistently apply existing knowledge in cancer control across all segments of the population, particularly to disadvantaged groups.”
Cancer Statistics has been published by American Cancer Society researchers since 1967 to inform and guide clinicians, investigators, and others in public health in prioritizing efforts to reduce the burden of cancer. It is one of the most highly cited scientific journal articles every year.
Article: Cancer Statistics 2017, Cancer J Clin 2017: doi: 10.3322/caac.21387.