Press Releases
“Future studies should examine patient-, clinician-, and health system–level factors to provide additional insight into the reasons for temporal changes and regional variation in the receipt of a CPM,” said Ahmedin Jemal, D.V.M., Ph.D., senior author and vice president of surveillance & health services research and the American Cancer Society. “In the meantime, however, surgeons and other health care professionals should educate their patients about the benefit, harm, and cost of a CPM to help patients make informed decisions about their treatments.”
March 29, 2017-- The proportion of women in the United States undergoing surgery for early-stage breast cancer who have preventive mastectomy to remove the unaffected breast increased significantly in recent years, particularly among younger women, and varied substantially across states. A new study co-led by the American Cancer Society and published in JAMA Surgery finds nearly half of young breast cancer patients in five states undergoing the procedure.
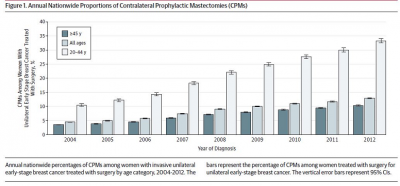
The use of contralateral prophylactic mastectomies (CPMs) among patients with invasive unilateral breast cancer has increased substantially during the past decade in the United States, particularly for patients younger than 45, despite the lack of evidence for survival benefit. The reasons for this increasing pattern are unclear but are thought to include the fear of developing a second breast cancer and the desire for breast symmetry following reconstructive surgery.
To find out more about this trend, investigators from the American Cancer Society, Emory University, Dana-Farber Cancer Institute, and Brigham and Women’s Hospital did a retrospective cohort study of 1.2 million women ages 20 and older who had been diagnosed with invasive unilateral early-stage breast cancer and treated with surgery from January 1, 2004, through December 31, 2012, in 45 states and the District of Columbia using data compiled by the North American Association of Central Cancer Registries.
Between 2004 and 2012, the proportion of patients who underwent a CPM nationally increased from 3.6% to 10.4% among women 45 and older and from 10.5% to 33.3% in those 20-44 years old.
While the increase was evident in all states, the magnitude of the increase varied substantially depending on the state. For example, among women ages 20 to 44, the proportion of CPM among women with unilateral early stage breast cancer and treated with surgery in New Jersey increased from 14.9% in 2004-2006 to 24.8% in 2010-2012, while in Virginia, the proportion tripled, from 9.8% to 32.2%.
Most strikingly, the proportion early-stage breast cancer patients age 20 to 44 receiving CPM in 2010-2012 were over 42% in the contiguous states of Nebraska, Missouri, Colorado, Iowa, and South Dakota.
From 2004 to 2012, the proportion of reconstructive surgical procedures among the women 20 to 44 increased in many states; however, that rise did not correlate with the proportion of women who received a CPM.
“Interestingly, the highest proportions of young women undergoing reconstructive surgery among young women who had a CPM were geographically clustered in several Northeastern states (Massachusetts, Maine, New Jersey, Connecticut, New York, and Delaware) rather than in the Midwestern region where we observed the highest proportions of women who underwent a CPM,” write the authors.
“Several previous studies in the United States have reported an increase in the use of MRI and high-risk genetic testing among patients with breast cancer, coinciding with the increase in the proportion of patients undergoing a CPM nationally,” write the authors. “However, the use of MRI and high-risk genetic testing among women is unknown by state, and we were unable to assess their contributions to the state variation in the proportions of CPMs among women with breast cancer treated with surgery.”
“Future studies should examine patient-, clinician-, and health system–level factors to provide additional insight into the reasons for temporal changes and regional variation in the receipt of a CPM,” said Ahmedin Jemal, D.V.M., Ph.D., senior author and vice president of surveillance & health services research and the American Cancer Society. “In the meantime, however, surgeons and other health care professionals should educate their patients about the benefit, harm, and cost of a CPM to help patients make informed decisions about their treatments.”
Article: State Variation in the Receipt of a Contralateral Prophylactic Mastectomy Among Women Who Received a Diagnosis of Invasive Unilateral Early-Stage Breast Cancer in the United States, 2004-2012 JAMA Surg. 2017;152(7):1-10. doi:10.1001/jamasurg.2017.0115 Published online March 29, 2017.